+++++++++++++++++++
Early attachment-relationship trauma and abuse changes us. When all is said and done, someday in the future, I believe researchers will arrive at a logical truth that I can see now — but they evidently cannot.
The research that would feed into the ‘proof’ I would need to ‘prove’ what I already know is just beginning to emerge in the fields of neuroscience, attachment, and infant-child development. Severe early attachment-related trauma, abuse, and neglect change the way the brain forms in response to PAIN. The brain changes the development of circuits that process information related to the developing-SELF-in the world.
The central processes of the brain involved in the see-saw process between rest and activity are directly tied to the nervous system process that relate to trauma-response and calm, relaxed connectedness – both to self and to others. There is — as will be shown — clearly definable trajectories of brain and nervous system changes that DID occur through early trauma within severely abusive people — including parents.
In the present moment fields of study that are beginning to define brain changes in both Borderline Personality Disorder and in schizophrenia that demonstrate these patterns. As I said in my earlier post, +IS THERE ANY OTHER WAY FOR ME TO ‘BE’ IN THE WORLD?, the concept of ‘coping mechanisms’ does not apply to infant-toddlerhood trauma and abuse survivors. The term ‘defense mechanism’ does not apply in the OLD way of understanding, either.
When early developmental trauma changes the molecular formation of the early body-brain, opportunities for CHANGE have to be considered in light of potential for conscious CHOICE. The more trauma was present during early development, the more developmental trajectories changed, the less potential there will be for consciously changing — at some magical later date — patterns of molecular operation in the body-brain. Wishful thinking does not abrogate this fact.
Researchers in the fields I mentioned are rarely interested in strictly defining the consequences of severe early infant-toddler and young childhood abuse, let alone in stopping these traumas from happening. I therefore find that reading the research that might hold the answers I am looking for is like performing delicate life-or-death surgery with a butter knife.
Defining the questions and looking for the answers about the causes and consequences of severe early trauma and abuse of infants and young children is an exercise in pandemonium. If I think in terms of the image of a triangle, I can see that research about so-called ‘mental illness’ and its so-called symptoms takes place near the point of the triangle’s top, nowhere near the ground zero supporting level of the line at the bottom where the causes and the consequences I am talking about actually take place — on the molecular level and in the very real world of unnecessary suffering that many, many people inhabit.
The further and deeper toward the supporting bottom of this triangle we look, the more cause and consequence of early abuse and trauma are connected. There is nothing glamorous about the kind of research-related thinking it will take to discover this truth.
Severe infant-toddler-young child abuse survivors currently exist within a category society considers to be ‘acceptable losses’. We are disposable and dispensable people. We were created within traumatic early environments that were themselves reflections of the kinds of circumstances those who abused us experienced in their own early lives. None of us are considered valuable enough to REALLY worry about.
We are left to survive mostly on our own, sometimes with supposed assistance from out dated, obsolete theories and treatments. There is a gross mismatch between what our needs truly are and what we are told are our solutions. Nobody is going to figure this out in my lifetime. That doesn’t stop me from trying to understand the rock-bottom truth about what happened to my mother that created the monster she was to me.
This post presents ‘pickings’ related to this topic. The stretch of thought that must happen to see how these bits of information relate to my topic takes effort. Nobody is going to do this work for us. All of us need to be encouraged to try. Again and again I have stated that from my point of view, informed compassion is the goal, not so-called forgiveness.
Our abusers were very REALLY hurt little people at one point in their lives when it mattered the most. They in turn hurt us during our developmental stages that in turn hurt us the most. This doesn’t mean that we must continue to miss the point about what these changes were and what they possibly mean.
+++++++++++++++++++
NEW CONCEPT — ‘first-person neuroscience’
How Does Our Brain Constitute Defense Mechanisms? First-Person Neuroscience and Psychoanalysis
Abstract
“Current progress in the cognitive and affective neurosciences is constantly influencing the development of psychoanalytic theory and practice. However, despite the emerging dialogue between neuroscience and psychoanalysis, the neuronal processes underlying psychoanalytic constructs such as defense mechanisms remain unclear.
One of the main problems in investigating the psychodynamic-neuronal relationship consists in systematically linking the individual contents of first-person subjective experience to third-person observation of neuronal states. We therefore introduced an appropriate methodological strategy, ‘first-person neuroscience’, which aims at developing methods for systematically linking first- and third-person data.
The utility of first-person neuroscience can be demonstrated by the example of the defense mechanism of sensorimotor regression as paradigmatically observed in catatonia. Combined psychodynamic and imaging studies suggest that sensorimotor regression might be associated with dysfunction in the neural network including the orbitofrontal, the medial prefrontal and the premotor cortices.
In general sensorimotor regression and other defense mechanisms are psychoanalytic constructs that are hypothesized to be complex emotional-cognitive constellations. In this paper we suggest that specific functional mechanisms which integrate neuronal activity across several brain regions (i.e. neuronal integration) are the physiological substrates of defense mechanisms.
We conclude that first-person neuroscience could be an appropriate methodological strategy for opening the door to a better understanding of the neuronal processes of defense mechanisms and their modulation in psychoanalytic psychotherapy.”
Copyright © 2007 S. Karger AG, Basel
++++++++++++++++++++
FROM: Deric Bownds’ MindBlog
His post — “Brain correlates of Borderline Personality Disorder”
Brownds’ article highlights the fact that the BPD brain does not process the human trust (oxytocin), cooperation and connection arm of the vagus nerve system in ordinary ways:
 (Click to enlarge). Activation of the anterior insula is observed during an economic trust game in individuals with borderline personality disorder and healthy controls. Both groups show higher activation in response to stingy repayments they are about to make. However, only players with the disorder have no differential response to low offers from an investor (upper left graph), indicating that they lack the “gut feeling” that the relationship (cooperation) is in jeopardy.
(Click to enlarge). Activation of the anterior insula is observed during an economic trust game in individuals with borderline personality disorder and healthy controls. Both groups show higher activation in response to stingy repayments they are about to make. However, only players with the disorder have no differential response to low offers from an investor (upper left graph), indicating that they lack the “gut feeling” that the relationship (cooperation) is in jeopardy.
++++++++++++++++++++
Research on trauma survivors of the Chinese Wenchuan 8.0 earthquake, demonstrated “a reduced temporal synchronization within the “default mode” of resting-state brain function.” READ ARTICLE HERE
This is the same brain area’s operation presented in this next article:
++++++++++++++++++++
Altered brain activity in schizophrenia may cause exaggerated focus on self
January 20, 2009 by Cathryn M. Delude
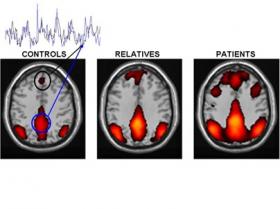
“Altered brain connectivity of default brain network in persons with schizophrenia and first-degree relatives. Colored areas represent an interconnected network of brain regions that show synchronized activity (overlapping black and blue traces) when subjects rest and allow their minds to wander. The amount of synchrony, which reflects the strength of functional connections between the different areas, is increased in patients with schizophrenia. First-degree relatives of persons with the illness also show some increase, although less than patients; this may reflect genetic effects on the brain that increase the risk of developing the disease. Black circle: medial prefrontal cortex. Blue circle: posterior cingulate/precuneus. Graphic courtesy: Susan Whitfield-Gabrieli
(PhysOrg.com) — Schizophrenia may blur the boundary between internal and external realities by over-activating a brain system that is involved in self-reflection, and thus causing an exaggerated focus on self, a new MIT and Harvard brain imaging study has found.
The traditional view of schizophrenia is that the disturbed thoughts, perceptions and emotions that characterize the disease are caused by disconnections among the brain regions that control these different functions.
But this study, appearing Jan. 19 in the advance online issue of the Proceedings of the National Academy of Sciences, found that schizophrenia also involves an excess of connectivity between the so-called default brain regions, which are involved in self-reflection and become active when we are thinking about nothing in particular, or thinking about ourselves.
“People normally suppress this default system when they perform challenging tasks, but we found that patients with schizophrenia don’t do this,” said John D. Gabrieli, a professor in the McGovern Institute for Brain Research at MIT and one of the study’s 13 authors. “We think this could help to explain the cognitive and psychological symptoms of schizophrenia.”
Gabrieli added that he hopes the research might lead to ways of predicting or monitoring individual patients’ response to treatments for this mental illness, which occurs in about 1 percent of the population.
Schizophrenia has a strong genetic component, and first-degree relatives of patients (who share half their genes) are 10 times more likely to develop the disease than the general population. The identities of these genes and how they affect the brain are largely unknown.
The researchers thus studied three carefully matched groups of 13 subjects each: schizophrenia patients, nonpsychotic first-degree relatives of patients and healthy controls. They selected patients who were recently diagnosed, so that differences in prior treatment or psychotic episodes would not bias the results.
The subjects were scanned by functional magnetic resonance imaging (fMRI) while resting and while performing easy or hard memory tasks. The behavioral and clinical testing were performed by Larry J. Seidman and colleagues at Harvard Medical School, and the imaging data were analyzed by first author Susan Whitfield-Gabrieli, a research scientist at the MIT Martinos Imaging Center at the McGovern Institute.
The researchers were especially interested in the default system, a network of brain regions whose activity is suppressed when people perform demanding mental tasks. This network includes the medial prefrontal cortex and the posterior cingulate cortex, regions that are associated with self-reflection and autobiographical memories and which become connected into a synchronously active network when the mind is allowed to wander.
Whitfield-Gabrieli found that in the schizophrenia patients, the default system was both hyperactive and hyperconnected during rest, and it remained so as they performed the memory tasks. In other words, the patients were less able than healthy control subjects to suppress the activity of this network during the task. Interestingly, the less the suppression and the greater the connectivity, the worse they performed on the hard memory task, and the more severe their clinical symptoms.
“We think this may reflect an inability of people with schizophrenia to direct mental resources away from internal thoughts and feelings and toward the external world in order to perform difficult tasks,” Whitfield-Gabrieli explained.
The hyperactive default system could also help to explain hallucinations and paranoia by making neutral external stimuli seem inappropriately self-relevant. For instance, if brain regions whose activity normally signifies self-focus are active while listening to a voice on television, the person may perceive that the voice is speaking directly to them.
The default system is also overactive, though to a lesser extent, in first-degree relatives of schizophrenia patients who did not themselves have the disease. This suggests that overactivation of the default system may be linked to the genetic cause of the disease rather than its consequences.
The default system is a hot topic in brain imaging, according to John Gabrieli, partly because it is easy to measure and because it is affected in different ways by different disorders.”
Provided by MIT
++++++++++++++++++++
Activation of Anterior Insula during Self-Reflection
This link describes yet another research study that links the brain default resting mode to self-reflection, a process that was seriously flawed in my borderline mother:
“The results provide further evidence for the specific recruitment of anterior MPFC and ACC regions for self-related processing, and highlight a role for the insula in self-reflection. As the insula is closely connected with ascending internal body signals, this may indicate that the accumulation of changes in affective states that might be implied in self-processing may contribute to our sense of self.”
++++++++++++++++++++
Processing of autobiographical memory retrieval cues in borderline personality disorder
Affective dysregulation [emotional dysregulation]in borderline personality disorder (BPD) in response to both external stimuli and memories has been shown to be associated with functional alterations of limbic and prefrontal brain areas….
Response “processing in BPD subjects were in line with previously reported changes in anterior cingulate and orbitofrontal cortices, which are known to be involved in memory retrieval. However, BPD subjects displayed hyperactivation in these areas … The deficit of selective activation of areas involved in autobiographical memory retrieval suggests a general tendency towards a self-referential mode of information processing in BPD, or a failure to switch between emotionally salient and neutral stimuli.
++++++++++++++++++++
I believe that emotional pain is as physiologically real as is physical pain. I also believe that the pain of malevolent early infant-child trauma, abuse and neglect creates changes in the developing brain that result in changes in these pain-reduction brain areas.
FULL ARTICLE FREE ONLINE:
Keeping pain out of mind: the role of the dorsolateral prefrontal cortex in pain modulation
“…the bilateral dorsolateral prefrontal (DLPFC) exerts active control on pain perception by modulating corticosubcortical and corticocortical pathways.” READ FULL ARTICLE HERE
++++++++++++++++++++
Dissociable Brain Mechanisms Underlying the Conscious and Unconscious Control of Behavior
— 2010 – Journal of Cognitive Neuroscience, MIT article
“Cognitive control allows humans to overrule and inhibit habitual responses to optimize performance in challenging situations. Contradicting traditional views, recent studies suggest that cognitive control processes can be initiated unconsciously….. [This research study presents]… patterns of differences and similarities between conscious and unconscious cognitive control processes are discussed in a framework that differentiates between feedforward and feedback connections in yielding conscious experience.”
+++++++++++++++++++++++++++++++
RESEARCH ARTICLE ABOUT CHANGES IN THE BORDERLINE BRAIN – CHANGES THAT MY MOTHER NO DOUBT HAD THAT CREATED HER ABILITY TO TORMENT, TORTURE AND TRAUMATIZE ME —
Please follow the active link for this title to read the full article including full references that I have omitted in these quotes below:
AUTHORS: Michael J. Minzenberg, Jin Fan, Antonia S. New, Cheuk Y. Tang, and Larry J. Siever
PUBLISHED: Psychiatry Res. 2007 August 15; 155(3): 231–243.
“…converging evidence suggests that the social and emotional disturbances of BPD may have a basis in the functional neuroanatomy of social/emotional information processing, supported by fronto-limbic circuitry….
“BPD patients exhibit a number of changes in the structure and function of subcortical limbic areas. This includes volume loss and lower resting metabolism in the amygdala and hippocampus … some studies have found amygdala volume to be preserved … The functional effects of this limbic pathology include elevated amygdala responses to emotional stimuli …and episodic memory deficits … which may be due to intrinsic hippocampal pathology or secondary to amygdala hyperactivity ….
“BPD patients also exhibit deficits in the structure and function of the rostral and subgenual subregions of the anterior cingulate cortex (ACC)…. The ACC may be a key neural region where altered processing of social and emotional information is expressed in some of the hallmark clinical signs of this disorder. The ACC is necessary for the maternal separation distress call of infant squirrel monkeys … and is activated in healthy adult humans both during the subjective experience of social rejection …and during effortful control of subjective emotional responses …. These experimental paradigms are related to clinical phenomena that are very characteristic of BPD, such as social attachment disturbance, rejection sensitivity and emotion dysregulation, respectively ….
+++++++++++++++++++++++++++++++
Neural paths for borderline personality disorder
People prone to stormy social lives display brain activity that may prompt oversensitivity to emotion and an inability to resolve conflicting information
By Bruce Bower
DOES THIS SOUND at all familiar?
“New brain-imaging research suggests that in people with borderline personality disorder, specific neural circuits foster extreme emotional oversensitivity and an inability to conceive of other people as having both positive and negative qualities…. Borderline personality disorder affects one in five psychiatric patients…. Most people have an important capacity for resolving conflict: the ability to perceive both favorable and negative aspects of the same person. Lacking this skill, borderline patients find it easier to veer back and forth between regarding those they know as either wonderful or awful….”
(My mother sure never ‘veered’ in her feelings toward me – no veering whatsoever! I was completely and totally ‘awful’ while the chosen good child, my sister, was the ‘wonderful’ one.)
+++++++++++++++++++++++++++++++
See also this post on the resting brain default mode:
+SOMETHING WENT TERRIBLY WRONG WITH MY MOTHER’S PRECUNEUS
++++++++++++++++++++
You must be logged in to post a comment.